~Ryan Joseph Smith~
My sisters, Joan and Julie, were in the labor room with us as well as Jim's parent's, Bob and Cheryl Smith. (Bob left just before Ryan made his appearance though. :-) Since the labor was so easy and pain free, we basically sat around chatting while the monitor showed the severity of the contractions I wasn't feeling. It was an extremely easy and uncomplicated birth... Looking back, we think that God gave us an easy birth so that we would have the emotional and physical energy to endure the complications that were just ahead.
Here I am with the Anesthesiologist getting the second shot in my epidural. Just 20 minutes before Ryan's birth.

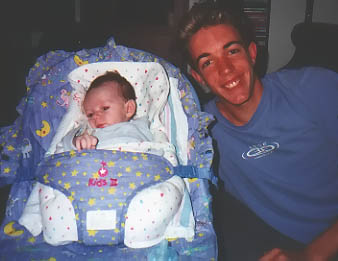
Welcome to the world Baby Ryan!
First photo with his Daddy and Mommy.

Jim with Grandma and Papa (Smith) holding their newest grandchild.
Aunt Joan...

...and Aunt Julie

What is Transposition of the Great Vessels/Arteries? The two "great" arteries of the body are the AORTA and the PULMONARY ARTERY. The aorta comes out of the left ventricle, and carries pure blood to the rest of the body. The pulmonary artery arises from the right ventricle and carries impure blood from the veins into the lungs for oxygenation. Transposition of the Great Vessels/Arteries - TGA, for short - as the name implies, means the two arteries are "transposed". That is, the aorta arises from the RIGHT ventricle, and the pulmonary artery from the LEFT ventricle.
Ryan was already across the street at CHOC having an emergency BALLOON ATRIAL SEPTOSTOMY performed on him to help regulate the flow of oxygen through the body until open heart surgery could be performed in a week.
What is a Balloon Atrial Septostomy? A catheter is a special thin tube passed into the blood vessels through a small needle-stick in the groin or forearm, and guided into the heart. Through this catheter, a special device that resembles a balloon is passed into the heart. The wall between the right and left atrium is punctured and the catheter device pushed through the small hole thus created. The balloon is then inflated, and the catheter is pulled back through the small hole, tearing it and making it larger. This procedure is called a Balloon Atrial Septostomy and was first devised by Dr.Rashkind. The aim is to create a large enough opening between the two atria, so that blood can freely mix across it, and improve oxygen supply.

Everyone entering the NICU must remove all jewelry and watches and scrub up for 3 minutes before entering. Children (if allowed in) must wear masks... Daddy helping Jake.
Getting the mask on Jake was an ordeal in itself :-)
24 hours later, the life of our precious bundle was in God's hands...
Jake was a little scared at the site of Ryan with so many iv's, but he tried to act like it didn't bother him.
The end of a long day...
August 26th...
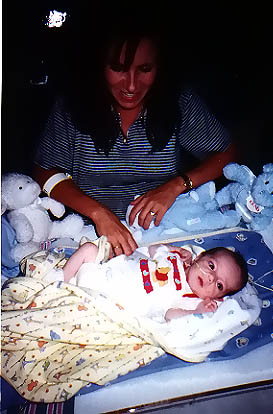
Very FIRST family photo with all four of us... Without the vent we are able to hold him finally!
Jill and Ron are 2 of many visitors that have arrived to see our little Ryan.
Ryan with his Daddy
Ryan with his Mommy and Daddy.
Ryan was baptized by a Catholic Priest. We knew that his chances for surviving were only 50%, so we wanted the chance to have him baptized.
Our favorite NICU nurse, Karen, helped us deal with the stress of the impending surgery the following day... Ryan loved Karen too!
How is an Arterial Switch Operation (ASO) done? Surgery is carried out through an opening in the middle of the chest. The heart will have to be stopped temporarily during the operation. So the surgeon will first hook up the patient to the heart-lung machine. The aorta and pulmonary artery are disconnected from their abnormal attachments. Their positions are then "SWITCHED". The aorta is stitched back to the left ventricle and the pulmonary artery to the right ventricle. A VSD is closed, if present. The coronary arteries are also freed, and connected back to the aorta using very delicate hair-thin sutures. When you consider that the size of these coronary arteries in a new-born is hardly a millimeter, you can imagine the technical skill and expertise that the surgeon must possess to carry out this connection without mishap.
Here is Ryan, our precious little miracle, in recovery hooked up to sooo many machines and IVs. Looking at this picture now horrifies me, but at the time, I didn't notice anything but my little angel lying there - still alive!
Grandma and Grandpa Smith visited often.
Ryan... so many iv's and lines keeping him alive...
Notice the 2 IV poles behind aunt Joan... Ryan had 11 IV's going at that point.
One of Ryan's favorite PICU nurses, Sharon, tries giving Ryan glucose water. His very first time trying to suck from a nipple... he wasn't very interested. :-) (Ryan's other 2 favorite nurses were Kathy and Bev... unfortunately we don't have photos of them)
Ryan in the PICU on September 19th, looking "oh so cute" in clothes for the first week!
October 8th, Jake and Ryan with their Mommy.
Grandpa and Grandma Harper, holding Ryan for the first time. (A memory I will always treasure...)
Aunt Mary...
Terry and Jim Ochoa... Terry is our children's daycare provider as well as a long time family friend.
Jim with Dr. Mike Rebolledo, Ryan's Cardiologist... checking out Ryan's heart before he could be discharged.
Patty Sheehan, Cardiac Clinical Nurse Specialist and long time family friend was truly there for our family through this horrible time. She gave us encouragement as well as her friendship when we needed her most. She was invaluable to us over the 7 weeks Ryan was in the hospital... always there for Ryan, even on her days off, with a smile, and a box of kleenex-lol!
Resident Dr. Melissa Rosin and Dr. Cleary checking Ryan's circumcision that he had gotten earlier that day before he could go home. Melissa was also an angel in disguise. She talked to us like we were friends and listened to our concerns about Ryan. She even held Ryan if he was crying and his nurse was busy.
Ryan's favorite Respiratory Therapist, Debbie!
October 13th, Just hanging out on the floor, relaxing with his Daddy.
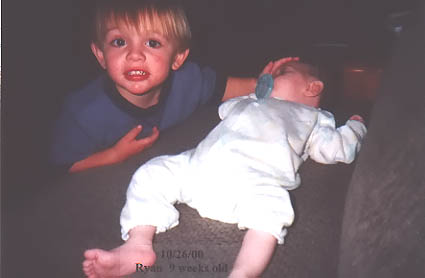
October 13th, Big Brother Jake and Ryan watching tv together.
October 14th, Ryan hanging out in his bouncy chair with his favorite cousin Brandon.
October 15th, Here we are at the CHOC WALK helping to raise money for the hospital that saved our Ryan's life.
Jake kissing his little brother.
October 26th, Jake, "Mr. Pacifier Police" himself making sure Ryan still had his pacifier in keeping him quiet.
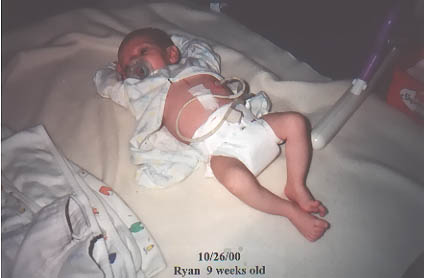
October 26th... Here's Ryan with his PEG tube in.
November 11th, at Grandma Harper's birthday celebration - Jake refused to take a picture with us...
How precious are those two?!!
Ryan went home on October 11th, 2000 with a Peg Tube in his stomach because he still wasn't eating enough from the bottle. Along with the PEG he was also taking several medications which included Methadone (to be slowly weaned off of), Reglan, Zantac, Iron, Lasix, Aldactone, Antibiotics and Tylenol several times a day. We were faced with a new challenge, learning to give medications through the PEG tube...
Once he got home, he refused to eat or be fed through the Peg-tube for the first week. It was a scary time, watching his progress regress... we talked to several doctors and, of course, Karin Mitchell regarding his feeding issues. Not only was he not eating, but he was crying constantly. We were told he had colic on top of everything else... but we couldn't help but think, "at least it's a NORMAL baby problem for a change!" We tried switching from breast milk to Similac formula to see if it made a difference on October 17th. Ryan's "colic" crying stopped with the formula switch. OVERNIGHT he started feeding again, but this time better than ever. A week later he was taking almost every feed from the bottle and not just the 55 required.
"I'm down on my knees again tonight. Can you hear me? Sometimes late at night I watch him sleep. Can you hear me?
Jim and Jake at the entrance to the NICU (Newborn Intensive Care Unit), a place that would become like home to us over the next several weeks.






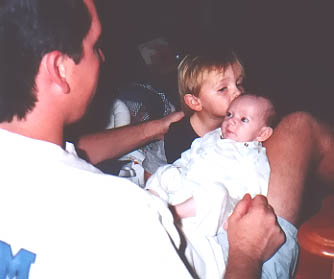
Jake sees Ryan again. This time he has been extubated (first of 4 times) so he is no longer on the ventilator.


In a meeting with Dr. Rebolledo, Cardiologist, Dr. Gates, Surgeon and Patty Sheehan, Cardiac Clinical Nurse Specialist (and family friend) August 28th, we learned that Ryan's heart defect was worse than first thought. We were told in that meeting that Ryan's chances of surviving the surgery were now 50/50. (I still tease Patty about walking into the meeting with a box of kleenex for me, that was a clue that there were complications.) After a long discussion regarding the surgery, we decided to go ahead with it and it was scheduled for August 30th. We knew that every moment we spent with Ryan from that moment on was going to be special because it could be our last. Unfortunately, Ryan was Re-Intubated that same day because his oxygen saturation level had kept dropping too low.







Ryan was moved to the PICU (Pediatric Intensive Care Unit-just across the hall from the NICU) on September 3rd after his chest was finally closed. Ryan had many visitors over in PICU...
Grandpa and Grandma Harper - their first of many visits with Ryan.



After 2 unsuccessful tries since Ryan's surgery, he finally was able to be extubated (taken off of the ventilator) for good! He wasn't actually "taken off" this time though... While he was being suctioned for excess fluids through his ventilator in his throat by his nurse Sharon, the vent just "slimed" out on its own. It wasn't scheduled to be taken out for days but he was fine without it so it stayed out for good this time. We were overjoyed to see Ryan's beautiful face without the vent! He did, however, still have an NG tube in his nose for eating. We were going to start trying to bottle feed Ryan the breast milk I had been religiously pumping later that evening.


Ryan and his Mommy... Ryan was transferred back to the NICU on September 22nd. There was talk about him being moved to the pediatric floor and out of ICU, but I begged Dr. Gates to let him stay in ICU until he was discharged. In peds he would have had less supervision and I wanted him to still have his own nurse. Since the PICU was filing up, Ryan was kept on the ICU floor and just moved to the NICU. It was actually better for him there anyhow, since we were working on teaching him to feed with a bottle and the NICU nurses are more trained to help babies with feeding issues. Being on the ventilator so long, Ryan was not able to suck, swallow and breath as a normal reflex during feedings. He could do all three, just not together. We began working with Karin Mitchell, Speech Language Pathologist, to learn how to deal with his feeding issues. From the day we started working with Karin, Ryan really started showing signs of improvement.

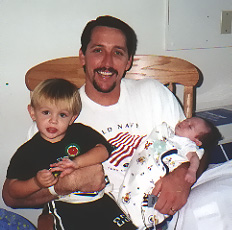
September 23rd, Jake and Ryan with their Daddy.




Ryan's PEG Tube was surgically placed into his stomach by Dr. Shaheen Idries, Gastroenterologist. Having the tube was the only way we could take Ryan home. Although he relied on it for some of his feedings, we were hopeful that he won't need to keep the PEG for long.


(Melissa Rosin has since become our pediatrician.)

Ready to go - smiling away in his carseat... what an angel!

Ryan in his bassinet at home, ready for bed... it's been a long 7 1/2 weeks...






While driving home from CHOC the night we found out Ryan had a 50% chance to live, this song came on the radio... I was crying, and the song made me stop and listen... the words were perfect, like my own personal prayer to God...
I'm hoping this prayer will turn out right.
See there is a boy that needs your help.
I've done all that I can do myself.
His mother is tired, I'm sure you can understand.
Each night as he sleeps, she goes in to hold his hand.
And she tries not to cry, though the tears fill her eyes.
Am I getting through tonight?
Can you see him?
Can you make him feel all right?
If you can hear me, let me take his place somehow.
See he's not just anyone, he's my son.
I dream of the boy he'd like to be.
I try to be strong and see him through.
But God who he needs right now is YOU.
Let him grow old, live life without this fear.
What would I be, living without him here?
He's so tired, and he's scared.
Let him know that you're there.
Can you see him?
Please don't leave him.
He's my son."